Abstract
Introduction: Active tuberculosis (TB) is an uncommon but life-threatening complication of haematopoietic stem cell transplantation (HSCT). HSCT recipients are at significant high risk due to their immunocompromised state either because of delayed immune reconstitution or use of immunosuppressive medication for treatment of GVHD. Early recognition and prompt treatment are the key to good outcomes in this patient population.
Methods:From January 2012 to December 2017, a nested case control study was carried out in our centre to examine active tuberculosis incidence and study relative risk factors. A total of 730 consecutive patients who underwent allogeneic HSCT were studied. Fourteen (1.92%) patients matched the established diagnostic criteria of active tuberculosis. Fifty-six allo-HSCT recipients were set as control. No significant difference was found between the two groups on age, gender, underlying disease, donor type and ATG given as well as conditioning intensity.
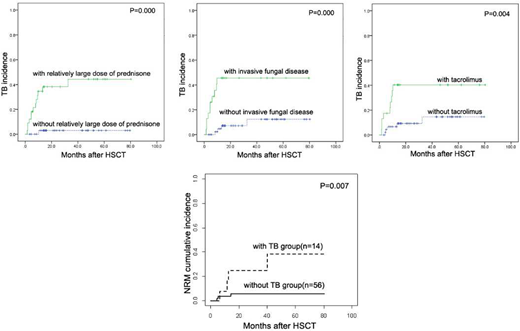
Results:Twelve of the fourteen cases were pulmonary TB (85.7%), including four patients with miliary TB, while the other two were extrapulmonary TB (14.3%). The median time to onset of active TB was the 6.9 (range 1.5 to 32.5) months post-HSCT. The positive rate of T-SPOT in patients with TB is higher than those without TB, the difference was statistically significant.(HR =6.286, 95% CI,3.093-12.774; P =0.000). We also found Grades 2 to 4 aGVHD (HR = 3.975, 95% CI, 1.331-11.876; P =0.013), moderate-severe cGVHD (HR = 3.952, 95% CI, 1.113-14.027; P =0.033), Epstein Barr virus viremia (HR = 9.210, 95% CI, 1.204-70.452; P =0.032), the application of etanercept (HR=3.928, 95% CI,1.375-11.220; P =0.011), invasive fungal disease (HR = 3.909, 95% CI,1.351-11.316; P =0.012), relatively large dose of prednisone (HR=17.831, 95% CI, 2.330-136.476; P =0.006), and tacrolimus (HR=4.340, 95% CI, 4.340-4.340; P =0.009) were risk factors for active tuberculosis occurrence, but only the latter three remained significant after multivariate analysis. Each of the prognostic factors was assigned points based on their HR: invasive fungal disease (1 point); the use of FK 506(1 points); or presence of relatively large dose of prednisone (2 points).This total score stratified the cohort into 3 groups with very different risk of occurrence of TB: low risk group ( 0 to 1 point), the intermediate risk group ( 2 to3 points) , and the high risk group (4 points). The 5-year cumulative incidences of active TB were 0, 30.7%, and 77.8% for each risk groups (p=0.001). With a median follow-up of 15.9 (range 3.8-80.6) months for patients with TB and 43.1(range 3.4-80.3) months for control group without TB, the 3-year OS were 68.1% and 70.0%, respectively. Subjects with TB had significantly higher 3-year none relapse mortality than subjects without (24.76%±13.37% vs 5.66%±3.22%, P=0.0076). The causes of death in TB group were engraftment failure/multi-organ failure (n = 1), and respiratory failure(n = 3).
Conclusions:Our study provides an excellent foundation for predicting of active TB occurrence in allo-HSCT recipients, and helps target high-risk patients for early diagnosis and timely management decision making.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal